How to cope with Chemo:
A personal Journey
My chemotherapy experience started out very challenging, but I learned how to make it better. Much to my surprise, I checked almost all of the boxes for possible side effects after my first infusion. I was strong, healthy, and young, so I thought it wouldn’t affect me that much. That is not how it turned out. My oncologist started talking about a dose reduction, but I wanted to make sure that I got the full dose and convinced myself that there was a better way of coping with side effects. I started to read advice from other survivors, finding out what helped them, as well as started doing my own research. By adapting new coping mechanisms with my second cycle, I experienced almost none of the side effects, much to my oncologist’s surprise! Suddenly, my chemo experience was so much better for all the consecutive cycles.
Want to know what helped me? Keep on reading below and remember DO NOT GIVE UP. There are things you CAN do and while my advice is personal, it serves as a valuable starting point for you to customize your approach. Everyone’s experience is unique, so take the time to read various blogs and gather the most helpful tips from each one. The regimen I was on was Taxotere and Cytoxan for four cycles, every three weeks.

12 Common Chemo Side effects and Coping Mechanisms
I only recommend products to help with side effects that I have personally used. If you click on the Amazon Affiliate Link, I may earn a commission.
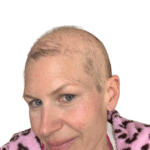
Chemo Hairloss
Going through breast cancer chemotherapy means that you will lose your hair, not only on your head but also on the rest of your body. My pubic hair and the hair under my arms fell out first. It was a perfect Brazilian wax and the best side effect of the treatment. My hair fell out right before my second cycle, approximately 17 days after my first infusion, which seems to be pretty common. Once I realized, while brushing my hair, that it had really started coming out in chunks, my friend came over, and we buzzed my hair to a nice buzz cut with an electric trimmer. The next day, while shampooing my hair, I could literally see what was left of my hair going down the drain! The buzz cut was okay, but being suddenly completely bald was hard! I am not going to lie, I mourned losing my hair more than my breast. At the very end, a month after my fourth and last cycle, to my surprise, even my lashes and eyebrows started to thin and fall out, even though my hair had already started to grow back.





Chemo Hair loss - What you CAN do
If keeping your hair is important for you:
- Cold capping: Lots of women report great results if done correctly. However, cold capping is not covered by insurance, so it can be expensive. It also prolongs your time in the chemo chair and can be very uncomfortable. You will need a helper or hire someone to help you exchange the cold caps. You will most likely experience an ice headache, which is quite painful. Watch my video about why I chose against cold capping.
- Wigs and scarfs. They are good alternatives if you won’t do cold capping. Ask your medical team to provide you with resources for wigs. There are a few great online resources where you can get a free wig or a free wig cap if you qualify. Click here to find more under Resources. As for head scarves, I used some that I already had. All major Cancer websites have tutorials how to properly tie headscarves. I ended mostly using beanies which were easy and kept my head warm. Those few times during chemo I did have the energy to go out, I wore my wig. I used a brow pencil to fill my brows the best I could. For those ladies ending up losing all their lashes, there are eyebrow stencils that are very helpful. There are also tutorials on all major breast cancer websites, f.eg. here.
- Lashes: Chances are you will lose some of them as well. I ended up with big gaps. Putting mascara on it just accentuated the gaps even more, so I used magnetic lashes.
- Eyebrows: Look into microblading. However, check with your doctor first because during chemotherapy you are more prone to infections and it should be done either prior or after treatment ends.



Neuropathy
Neuropathy is when nerves get damaged, causing feelings of pain, tingling, or numbness. The nerves that send signals from your brain and spinal cord to other parts of your body make up your peripheral nervous system. When these nerves get damaged, it is called peripheral neuropathy. It usually starts in your hands and feet. Chemotherapy can also cause peripheral neuropathy, which is called chemotherapy-induced peripheral neuropathy. During breast cancer treatment, Taxol or Taxotere are often used along with other medications. For me, Taxotere and Cytoxan had neuropathy listed as a possible side effect.
Neuropathy - What you CAN do
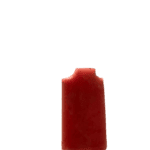
Cryotherapy: This involves applying frozen mittens and socks or cold packs to the hands and feet while receiving chemotherapy. Icy cold hands and feet are no fun and you won’t be able to do anything with your hands to pass the time. However, for me it was worth it. I believe the key is to be consistent. Luckily, I never experienced neuropathy and believe cryotherapy works. It also helps save your nails; mine remained strong and healthy.
I tested several ones and these mittens and these socks work in my opinion the best. Here is how you will use them:
Test your mittens and gloves at home: See if you need a few additional layers to tolerate the cold therapy. I personally could not tolerate the ice boots or gloves without additional layers. I got some thin cotton gloves and some thick socks that I was wearing under the booties and mittens as a protective layer and shed them as they warmed up.
Calculate the number of required booties and mittens: Ask your medical team how long your infusion will take approximately. Then calculate the number of required booties and mittens (the manufacturer will state how often they should be changed) and add 1 or 2 replacement packs for your mittens and booties. Get your replacement mittens here and your replacement booties here.
Put your mittens and boots in your freezer two days prior to your infusion.
On Infusion Day: Bring them in an ice chest to the infusion center and apply ice mittens and socks 15 minutes before the infusion starts, and keep them on 15 minutes after the infusion ends.
Remember, your hands and feet must be as cold as you can tolerate! If you need a break, take one, you don’t want to get frostbite. My mittens and booties remained cold for about 45 minutes. Every 45 minutes I swapped them with a new pair that I stored in the ice chest that I brought to the infusion.
Dress in warm clothes: You will be cold! I highly recommend you bring a hot water bottle to put on your lap. It will stay warm for a long time. Also, bring along a warm blanket or an electric blanket.


Chemo Mouth Problems
There are quite a few oral issues that may arise. Your mouth can get infected, sore and swollen, very dry and you may experience trouble swallowing. Some women experience a change of taste and smell. As a consequence of the lack of saliva, cavities can form. Dry lips are also common.
With my first cycle, I experienced almost all of the side effects. After day 7 of my first infusion, I had a swollen throat, swollen tonsils, trouble swallowing, mouth sores, and my mouth constantly felt like having a dirty sock in my mouth because it was so dry!


Chemo Mouth Problems - What you CAN do
Oral hygiene during chemo is very important.
Schedule a dentist appointment before your chemo starts: Tell the dentist about your cancer treatment and try to get any dental work completed before starting treatment.
Check your mouth every day for sores or white spots.
If you get mouth sores, apply some milk of magnesia with a Q-tip: It worked quite well for me. Don’t forget to check with your doctor.
Rinse your mouth throughout the day with a solution of warm water, baking soda, and salt: Ask your nurse to write down the mouth rinse recipe that is recommended for you.
Use soft toothbrushes to brush your teeth, gums, and tongue after each meal and before going to bed at night.
Use a Waterpik instead of dental floss if you experience bleeding.
Get yourself some Biotene Products: Biotene Toothpaste, and a Kit containing Biotene Gel, Spray and Mouthwash and lozenges. They do help with your dry mouth.
Consider applying fluoride varnish once a week to prevent cavities: Check with your dentist.
Cold therapy works for your mouth as well: Consider sucking on ice and popsicles during your infusion. I started doing that for all the consecutive infusions and I didn’t experience ANY of the mouth problems I had experienced the first time. Start sucking on ice chips 15 minutes before the infusion and 15 minutes after the infusion ends. You will need a helper that will feed you the ice chips, especially if you choose to also do the ice mittens.




Chemo GI Issues



Chemo GI Issues - What you CAN do
- Don’t underestimate the power of food.
- The better you hydrate and nourish your body, the better you will tolerate Chemo. When you go into Chemo, you will most likely get educated about eating small frequent meals, getting enough fiber, and choosing lightly digestible foods, especially during the days leading up to chemo and the days after. However, I have been eating healthy my whole life and that advice still didn’t cut it for me.
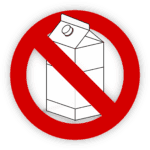
- If you experience severe GI Issues, experiment by cutting out dairy. It solved most of my GI Issues. Why? Simply because I became lactose intolerant, which I wish I had known before going into Chemo that it could be a possibility. My oncologist explained that the enzyme to process lactose is in the lining of stomach which are fast dividing cells that get destroyed by chemo drugs, thus destroying the enzyme, as well. It all made sense to me now. Unfortunately, I learned that after suffering many painful bouts of cramps and sleepless nights. So watch out for that possibility!
Here is what worked best for me to fix all of my GI Issues by eating the following foods the night before Chemo, the evening after the infusion, and the following two days after.
- Dinner and lunch: Overcooked white rice with chicken breast and grated ginger.
- Breakfasts consisted of plain porridge, sometimes toast and a little scrambled egg. If I was hungry, I snacked on plain crackers and sipped on homemade bone broth.
- During the Infusions: Steamed purple yams.
- I exclusively drank water, as well as fennel and ginger teas.
I was sick after a few days of eating the same chicken, rice, and ginger combo, but I felt so much better sticking to these simple foods. As the days went on, I very slowly introduced a bigger variety of food. But I would stick to fairly blend and nutritious foods. Only after 10 days I would resume a more normal diet, however paying attention to basic principles, such as lightly digestible foods, smaller and frequent meals, nothing fried or heavy, neither alcohol or coffee. Never underestimate how properly nourishing your body can make a big difference!





Chemo Skin Changes
Chemo dries your skin out and may make it more sensitive to sunlight. You may develop flushing (red cheeks), hives, and rashes as a reaction to your Chemo drugs. Flushing occurs due to the steroids that are administered before the actual Chemo Cocktail. Once you start taking steroids, it’s common to have a red face. Around 10 days after my infusions, I experienced all kinds of weird rashes on my neck, pimples on my back, and ultimately on my scalp, as well as hives on my arm. With the last two cycles, I also developed rosacea.




Chemo Skin Changes - What you CAN do
Moisturize regularly with gentle, fragrance-free lotions.
Use a gentle, hydrating cleanser.
Avoid hot showers or baths, which can dry out your skin.
Wear sunscreen to protect your skin from the sun.
Consult your doctor if you notice any severe skin reactions.
- Consider swapping to personal care products that are free of toxins and fragrances. I highly recommend using the apps EWG, Think Dirty or Clearya to access ratings about toxins in common foods, personal care and cleaning products.
- Be patient with your skin: all my skin problems with proper care started to fade be about two month after ending my last infusion. To control the Rosacea took a little bit longer. After 6 months my skin looked just as healthy as before.


Chemo Fatigue
I didn’t really understand what cancer fatigue was until I experienced it myself. Just the feeling of being completely worn out once all the steroids that are given to you as premeds wear off, and then the few days following your infusion. I had days where going to the bathroom or even taking the blanket off of me in bed felt like too much work! Usually, your energy levels get better as you get closer to your next infusion. However, as treatment goes on, often fatigue tends to build up. Everybody is different, and for me, my fatigue was the most pronounced after my first infusion because I suffered the most side effects. All the following infusions were much easier. Read below to find out what helped me to beat fatigue.
Chemo Fatigue - What you CAN do
- Commit to gentle movement and listen to your body, being mindful of your side effects. After my first infusion, I was too weak to get out of bed. But once I conquered diarrhea, I pushed myself to walk and found that my fatigue improved. Walking is a great exercise during treatment. After your Neulasta shot, your body may ache and walking may be challenging. But you’ll feel better if you can manage it, and stretching is a good alternative.
- Adjust your pace to reflect your energy levels: Some days you may be more fatigued than others, so take shorter walks at a slower tempo.
- Invite a friend to join you: Walking with a friend whom you enjoy talking to will help you avoid feeling isolated. It will also contribute to your overall well-being.
- Boost your energy with beet juice: After my first cycle, I began drinking beet juice daily and found that my energy levels increased throughout my treatment. The nitrates naturally occurring in beets help to open up blood vessels so that more oxygen and nutrients can reach the muscles, making it easier for athletes to maintain high workloads for longer periods. Give it a try and see if it works for you!
For your juicer you only need 3 ingredients: Apples, Beets, and Carrot (ABC Juice) . Try to add Ginger.
Add the fruit in equal quantities and the Ginger to your taste.

The picture below was taken on day 7 after my fourth infusion. I hiked for 3 miles with my dogs, going up and down hills.



Chemo Bone and muscle pain
You may experience muscle and bone pain from chemotherapy drugs. Taxotere and Taxol often cause these side effects. The white blood cell growth stimulants, Neulasta or Neupogen, may also make you feel achy. It feels like having a bad flu with body aches. The first time it really hurt, but I eventually learned how to handle it without having to take Tylenol.
Chemo Bone & Muscle Pain - What you CAN do
- Talk to your health care team: They suggested to take Claritin or Zyrtec, the day before and the following five days after the Neulasta shot. For me, Zyrtec worked best, so experiment with what works for you.
- Try Epsom salt baths, massages, foam rolling, and stretching. Self-care is very important, not only for your physical, but also mental, well-being.
- Find the right combination of self-care practices to support your body and mind: Remember, you are in control of your health journey.



Needle anxiety
I didn’t realize that getting chemotherapy automatically means you are getting poked with a needle repeatedly. Your oncologist will check your blood before each infusion. Then, you will receive an IV to administer your chemo drug. Then, before your next cycle, your oncologist will check your blood again to evaluate if your values are okay to receive the next cycle. In between, you will receive either one injection to stimulate your white blood cells if you have the Neulasta shot, or you will receive several daily injections if you receive Neupogen. (Note that there is an alternative for the injection called Neulasta Onpro, which is a patch instead of an injection). If anything is off and you develop symptoms such as a fever, the first thing your medical team does is take a look at your blood.


Needle Anxiety - What you CAN do
- Ask your oncologist about the option of a port: There are advantages and disadvantages of having one. Since I only had 4 infusions, I opted against it.
- Ask for EMLA cream: It numbs your skin and it significantly decreases the pain of blood draws and IVs. Since you won’t know which vein your nurse will use, smear the cream thick on your whole underarm at least 60 min. before your infusion or blood draw and cover it with clear kitchen wrap. Maybe your nurse will laugh at you but let them!
- Use mindfulness practices to be more calm before the infusion: Use an app like “Calm” or “Insight Timer” and choose meditations to release anxiety. Diaphragmatic Breathing techniques also help to release anxiety during the time the placed the IV and it helped. Watch this Video for Diaphragmatic Breathing.




Hotflashes and Nightsweats
Premenopausal women like me, will experience medically induced menopause due to chemotherapy. Hot flushes, often at night, are expected and may cause excessive sweating that requires changing of pajamas multiple times. Night sweats and disrupted sleep may start after the first infusion and worsen with the third, causing exhaustion during the day.
Hotflashes & Nightsweats - What you CAN do
- Get a buckwheat pillow: I use one until this day, which didn’t leave me with the feeling of my head burning up on a hot pillow. There are also cooling pillows that you can buy.
- Invest in cooling bedding: I found cooling bamboo sheets and a 100 percent cotton mattress protector useful.
- Consider putting a fan by your night stand.
- Talk to your doctor about medications that can help with Hot flashes.
- Be patient: experiment what works for you.
If you had an estrogen receptor positive breast cancer, your doctor will be prescribing you endocrine therapy to prevent recurrence. You will stay in a prolonged menopause even after finishing your treatment. If you want to find out more about managing menopausal symptoms and how I learned to cope with them click here.
Depression and Anxiety
Chemotherapy can take a toll on your emotional health. There are things that helped me strengthen my spirit and get through the treatment. Read more below:
Depression & Anxiety - What you CAN do
- Take inspiration from survivors: Learn everything from other survivors who had your cancer and were at the other end of the treatment and are now living their best life.
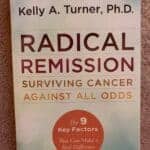
- Check out the book “Radical Remission: Surviving Cancer against all Odds” – it is a must-read in my opinion. This uplifting book shares the stories of those who have defied convention and survived against all odds. There are nine factors that lead to spontaneous remission from cancer, and this book explores them all. It’s truly inspiring to read and will give you the strength to believe that you, too, can overcome any obstacle in your path.
- Listen to podcasts of women who have gone through the same process. I liked the podcasts “Rotten Melons” and “Besties with Breasties”. These incredible women share their journey and provide hope and optimism for those going through this difficult time.
- Watch the movie “HEAL”, which takes you on a scientific and spiritual journey, demonstrating that the power of the human mind can play a significant role in overcoming any disease.
So let these inspiring survivors remind you that anything is achievable if you believe in yourself.
Click here to find more under the Resource section
- Keep moving, it will lift your spirit! Exercise is the best free antidepressant. Think that even a few minutes is better than not moving. Personally, I enjoyed to go for walks with friends and being outdoors. I always felt better.
- Make an effort to surrounded yourself with people who are supportive and uplifting, and cut out negative unsupportive people. You will notice a big difference because you will rather feel connected and not isolated by your treatment.
- Look for Traditional therapy and/or private healing sessions. I highly recommend to look at the amazing resources the organization Docancer provides for cancer patients. You will get free access to very talented therapists. Their traditional therapist is a breast cancer survivor herself and I cannot recommend her enough. Click here to find more information about my experience with DoCancer (coming soon).
- Start a gratitude journal and write down 3 things you are thankful for daily. It doesn’t have to be complicated, you could be thankful for being able to play a game with your children or drink a cup of tea.
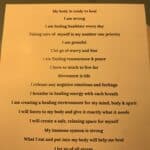
- Using daily positive affirmations were an integral part of reducing my post active treatment anxiety. I kept telling myself everyday: ” Your body has the ability to heal”, “Your immune system is strong” and “I let go of worry and fear”. Choose your mantras and go by it.
- Integrate meditations into your daily routine. It can help you to manage your stress and decrease your anxiety. It can be as simple as pausing during the day and taking deep breaths.



Being Immunocompromised
Chemotherapy is a treatment for cancer that can weaken your immune system because your white blood cells are also affected. It’s much easier to contract an infection if you don’t have enough of them. The Neulasta or Neupogen shot can help with this, but you’ll still be more vulnerable to illnesses during Chemo. Of course, it doesn’t help to have toddlers and young children since they’re often sick, particularly during the fall and winter months. That’s when my Chemo began, right before the Thanksgiving holiday. I asked my oncologist how I could possibly endure Chemotherapy with young children bringing all sorts of germs home. Giving up or not having Chemo is not an option. Find out what you can do!
Being Immunocompromised - What you CAN do
- Protect yourself: be consistent in having everyone in your family wear a good mask, and let your visitors know, too.
- Have hand sanitizer handy and practice good hand washing.
- In case of Illness: keep your a distance and have your partner care for the sick child. If we had kids’ birthday parties, I sent my family masked while I was healing at home.
- Meet with your friends outside unmasked if the weather permits.
It will be hard to be consistent with young children, but if you persist, it will pay off without delaying any infusion and extend the duration of chemotherapy. Your children will eventually get used to it. I never caught a cold or any illness during that time and had started chemotherapy the week before Thanksgiving.
Chemo Allergic Reactions
You may or you may not have an allergic reaction to your Chemo drugs. Allergic reactions can happen during the infusion or even later. Taxotere caused me twice to have an allergic reaction. Each time the nurse started to increase the drip I turned red, my heart started racing, I felt nauseated and couldn’t breath. I am not going to lie, it was awful!
Chemo Allergic Reactions - What you CAN do
- Knowledge is power: If you know this can happen, you will know to alert your nurse right away should it happen to you. Sadly, cost always plays a roll and your care team will want you rather sooner than later out of the chemo chair.
- Always listen to your body and don’t stop advocating for yourself!
Conclusion
Chemotherapy is a challenging journey, but there are many ways to cope with the side effects. By following these tips and working closely with your healthcare team, you can manage the side effects more effectively and improve your overall well-being. Remember, every person’s experience with chemotherapy is unique, so find what works best for you and don’t hesitate to seek support when needed.
I hope this helps, and if you have any questions or need further information, please feel free to reach out. Stay strong and take care!
Join Our Community
If you found this guide helpful, please share it with others who might benefit. For more detailed information, personal stories, and expert advice, subscribe to my newsletter [Subscribe Now].
Follow Me on Instagram
For weekly inspiration, tips, and updates, connect with me here!
Thank you for being a part of our community.

